Photos: Kaylee Pugliese (left) - Bryan Goodchild (right)
An entirely virtual community health intervention called Home Test to Treat that provided free COVID-19 at-home rapid tests, telehealth sessions and at-home treatments demonstrated the effectiveness of telehealth in reaching vulnerable populations and providing care outside of business hours, according to UMass Chan Medical School researchers involved in the program.
Home Test to Treat was launched initially as a pilot in Berks County, Pennsylvania, in January 2023, as a federal response to improve access to COVID-19 testing and treatment after reports that rural or otherwise underserved communities were having difficulty accessing care.
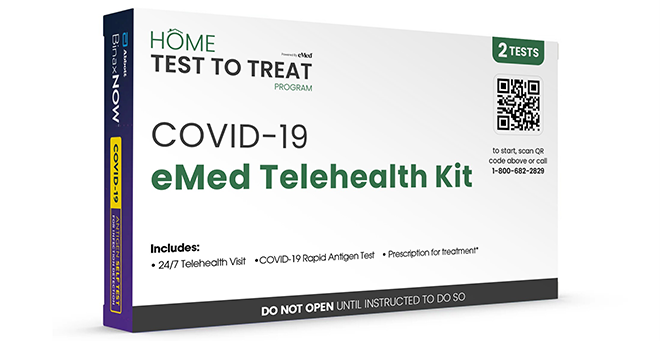
Participants could receive free COVID-19 tests sent to their home. If they tested positive, they were offered a telehealth consultation and, if indicated, receive a prescription for oral antiviral medication delivered to their home or available to be picked up.
Informed by what was learned in Pennsylvania, the program was launched in Houston and Atlanta in August and September 2023. It expanded nationally in fall 2023.
Home Test to Treat is a collaboration among the National Institute of Biomedical Imaging and Bioengineering, Administration for Strategic Preparedness & Response, Centers for Disease Control and Prevention, UMass Chan Medical School, VentureWell, and eMed.
“We need to do more in terms of reaching populations more equitably, but by and large, what we found was we were able to overcome some of the historical and well-identified barriers to care,” said principal investigator Apurv Soni, MD, PhD’21, assistant professor of medicine and co-director of the Program in Digital Medicine at UMass Chan. Dr. Soni and others shared their findings and lessons learned in a webinar on Jan. 16.
As the program launched following the pilot, a community engagement team was brought on to help with outreach to hard-to-reach communities, including those with language or cultural barriers. Organizers also worked with local government departments, national and community-based nonprofit organizations, community health centers, faith-based organizations, and social media to spread a wide net for enrollment.
Soni said the program surpassed its enrollment goal of 60,000. More than 100,000 people expressed interest in Home Test to Treat; more than 80,000 enrolled; more than 40,000 received tests at home; more than 10,000 tested positive for COVID-19; 8,000 received telehealth; and more than 6,000 were prescribed oral antivirals such as Paxlovid.
Among those who received telehealth, 76 percent of their consultations occurred outside of normal business hours. And 60 percent of those who were prescribed oral antivirals got their prescription within one day of symptom onset, which is within the five-day timeframe when the drugs are most effective.
In December 2023, the program expanded to include testing and treating for flu. According to the Home Test to Treat website, it ended in April 2024.
“Two themes that I want to highlight are the scale and the rapidity with which the program was implemented,” Soni said. “A lot of this happened over a period of really eight to nine months.”
Soni added that the program reached people in more than 98 percent of the ZIP-three regions (the first three digits of a ZIP code) of the country, including Alaska and Hawaii. These areas include regions with a shortage of health care professionals.
Kimberly Fisher, MD, associate professor of medicine and study lead of qualitative evaluations, reported on interviews she conducted with a subset of participants who received telehealth.
“A real strength and benefit of the Home Test to Treat project is really widespread access with no barrier to getting care for a significant problem,” said Dr. Fisher.
She said patients liked the convenience and ease of getting care on a weekend or if they were away on vacation.
Fisher said the model offered advantages to physicians because much of the telehealth for patients could be handled by other clinical staff. However, she emphasized the importance of coordinating patients’ telehealth with primary care physician practices, especially for patients with complex needs, to ensure there is continuity of care.